Contents
PPO vs. HMO: Complete Guide to Dental Insurance in the United States
The US dental insurance market is experiencing exceptional growth. Valued at over $90 billion in 2024, it is projected to more than double by 2034, reflecting a growing public awareness of oral health's importance. In this dynamic context, understanding the fundamental differences between the two main types of dental plans—PPO and HMO—is crucial for making an informed decision that impacts both your access to care and your budget.
The Core Choice: Cost vs. Flexibility
Choosing between a PPO (Preferred Provider Organization) and an HMO (Health Maintenance Organization) dental plan boils down to a single, critical trade-off: paying more for flexibility or saving money with a more structured network. PPO plans overwhelmingly dominate the market, accounting for over 80% of all commercial dental plans, precisely because they cater to the American consumer's preference for choice.
Dental PPO: The Power of Choice
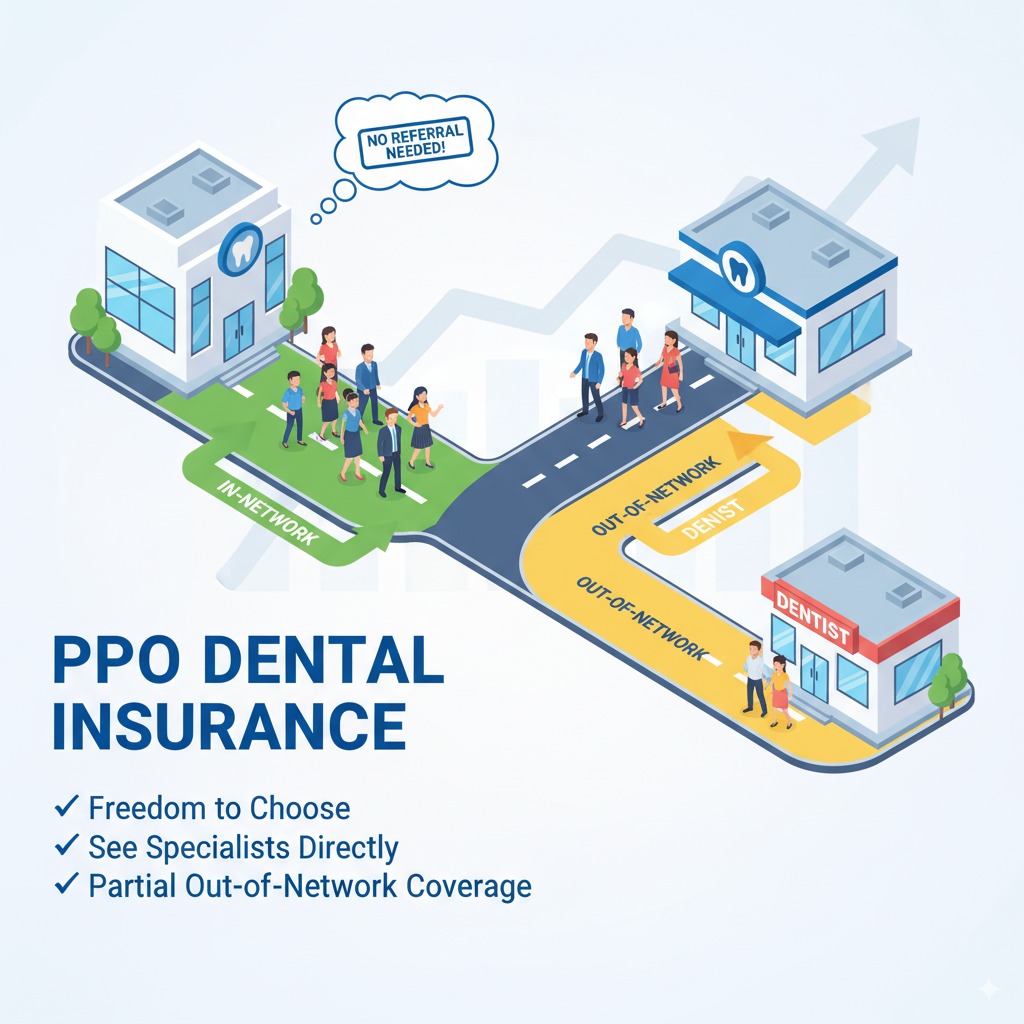
A PPO plan is built around a network of "preferred" dentists who have agreed to provide services to plan members at a discounted, pre-negotiated rate. Its defining feature is the freedom it offers.
Key Features of a PPO Plan
- Freedom to Choose Your Provider: This is the main advantage. You can see any dentist you like, whether they are in-network or out-of-network.
- Out-of-Network Coverage: If you visit an out-of-network dentist, the PPO plan will still pay a portion of the cost, though your share (coinsurance) will be higher than if you stayed in-network.
- No Referrals Needed: You do not need a referral from a primary care dentist to see a specialist like an orthodontist or periodontist, giving you direct access to specialized care.
The Financial Trade-Offs
This flexibility comes at a price:
- Higher Monthly Premiums: PPO plans are consistently more expensive than HMOs.
- Deductibles: You must typically pay an annual deductible (often $50 for an individual, $150 for a family) out-of-pocket before your insurance starts to pay.
- Annual Maximums: Most PPO plans have a yearly limit on what they will pay for your care, typically ranging from $1,000 to $2,500.
Dental HMO (DHMO): The Budget-Friendly Option
A Dental HMO (often called a DHMO) operates on a managed-care model designed to be more affordable by restricting your choice to a specific network of dentists.
Key Features of an HMO Plan
- Lower Premiums: HMO plans have significantly lower monthly costs, making them a budget-friendly option.
- No Deductibles or Annual Maximums: Most HMO plans have no deductible to meet and no yearly cap on benefits.
- Predictable Copayments: Instead of percentages, you pay a fixed, predictable copayment for each service (e.g., $25 for a cleaning, $150 for a filling).
The Trade-Offs for Lower Costs
- Limited Network: You MUST use a dentist from the plan's network to receive any coverage. There is no out-of-network benefit.
- Primary Care Dentist (PCD) Requirement: You must select a primary care dentist from the network who will act as a "gatekeeper" for your care.
- Referrals for Specialists: You will need a referral from your PCD to see a specialist, which can add an extra step to the process.
Head-to-Head Comparison: PPO vs. HMO at a Glance
| Feature | Dental PPO | Dental HMO (DHMO) |
|---|---|---|
| Monthly Premium | Higher | Lower |
| Provider Choice | Choose any dentist (in or out-of-network) | Must use in-network dentists only |
| Deductible | Yes, typically $50-$150 | Usually none |
| Annual Maximum | Yes, typically $1,000-$2,500 | Usually none |
| Referral to Specialist | Not required | Required |
Market Trends: What's Shaping Dental Insurance in 2025?
The US dental insurance market is evolving rapidly. The growing use of teledentistry for consultations and follow-ups is being integrated into many plans, offering new convenience. Furthermore, there is a strong trend towards plans that emphasize preventive care, often covering cleanings and exams at 100% to help reduce the need for more costly major procedures down the road.
How to Choose the Right Plan for You
Choose a PPO if...
- You already have a dentist you love and want to continue seeing them, regardless of their network status.
- You anticipate needing specialized care and want direct access to specialists without a referral.
- Your budget allows for higher monthly premiums in exchange for greater freedom.
Choose an HMO if...
- Your primary concern is keeping monthly costs as low and predictable as possible.
- You are comfortable choosing a dentist from a provided list and getting referrals for specialists.
- You mainly need preventive and basic care and want to avoid deductibles and claim forms.
Conclusion: A Strategic Decision for Your Health and Wallet
Ultimately, there is no single "best" plan; the right choice depends entirely on your unique needs. DHMO plans are more cost-effective for predictable budgeting, while PPO plans offer unparalleled flexibility at a higher cost. In a rapidly growing market, understanding this core trade-off is the key to selecting a plan that aligns with your financial priorities, lifestyle, and dental care needs.
FAQ: Your Top PPO vs. HMO Questions Answered
Yes, in terms of monthly premiums, PPO plans are almost always more expensive. However, the total annual cost can depend on your usage. If you need extensive care from an out-of-network provider on a PPO plan, your total out-of-pocket costs for the year could potentially be higher than with an HMO where costs are fixed.
A waiting period is a set amount of time you must be enrolled in a plan before certain benefits become active. It's common for PPO plans to have a 6 to 12-month waiting period for major procedures like crowns or implants to prevent people from signing up only when they know they need expensive work done. HMOs and group plans through an employer often do not have waiting periods.
Yes, one of the major advantages of a PPO plan is its geographical flexibility. Most PPO plans have large, nationwide networks, and even if you find yourself needing care from a dentist who is out-of-network in another state, you will still receive out-of-network coverage. An HMO plan's coverage is typically restricted to a specific service area.
