Contents
Pre-Authorization Requirements for Dental Insurance: 2025 Complete Guide
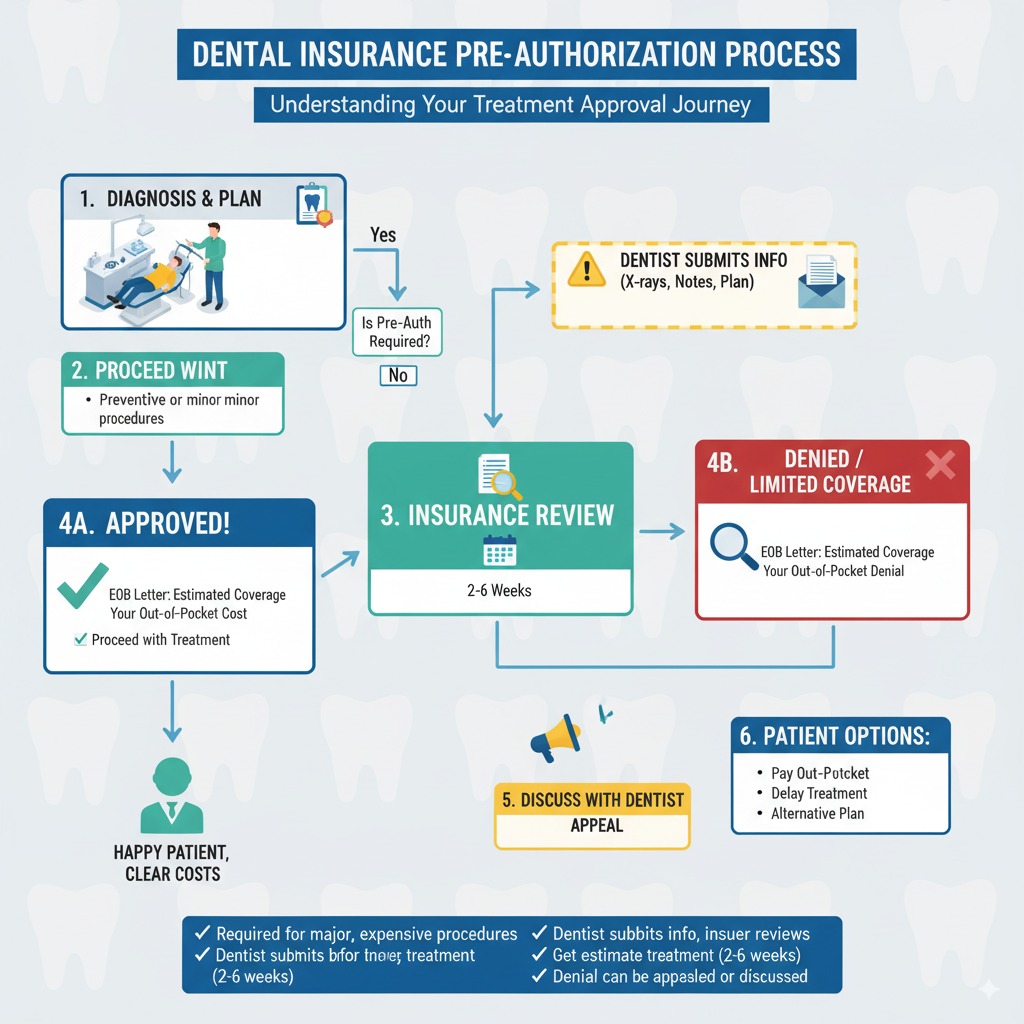
Pre-authorization, also known as prior authorization, is a critical process in which your dental insurance company must review and approve a proposed treatment before you receive it. As insurers seek to manage costs and ensure medical necessity, this requirement has become increasingly common. With significant regulatory changes speeding up review times in 2025, understanding how to navigate this process is more important than ever for patients and dental providers.
What is Dental Pre-Authorization and Why Does It Matter?
Pre-authorization is a cost-control measure that verifies a procedure is medically necessary and covered under your plan's terms. For you, the patient, it provides financial certainty. An approved pre-authorization is a confirmation from your insurer that they will pay for the procedure, helping you avoid unexpected, large bills. For your dentist, it ensures they will be properly reimbursed for their services.
Common Procedures That Require Pre-Authorization
Insurers typically require pre-authorization for expensive, complex, or elective procedures. While requirements vary by plan, they almost always apply to:
- Major Restorative Work: Crowns, bridges, dentures, and especially dental implants.
- Surgical Procedures: Complex extractions (like wisdom teeth), periodontal (gum) surgery, and bone grafts.
- Orthodontic Treatment: Both traditional braces and clear aligner therapy (e.g., Invisalign).
- Specialized Treatments: Sleep apnea appliances, TMJ treatments, and extensive treatment plans that exceed a certain dollar amount (e.g., over $500).
The Pre-Authorization Process: A Step-by-Step Breakdown
The process is handled almost entirely by your dentist's office. Here’s what it involves:
- Submission: Your dentist submits a detailed treatment plan, including specific procedure codes (CDT codes), X-rays, clinical photos, and a letter explaining why the treatment is medically necessary.
- Review: A clinical consultant at the insurance company reviews the documentation to ensure it meets the plan's criteria for coverage.
- Decision: The insurer issues a decision. As of 2025, new CMS regulations for many plans require a decision on standard requests within 7 calendar days. The decision will be an approval, a denial with reasons, or a request for more information.
Pre-Authorization vs. Predetermination: A Crucial Distinction
Pre-Authorization
This is a mandatory process for certain procedures. It is a formal approval that guarantees payment if all conditions are met. Think of it as getting a green light before starting a race.
Predetermination
This is a voluntary process, also called a pre-treatment estimate. It provides an estimate of what your plan will pay but is not a guarantee of payment. It's like checking the weather forecast before a trip—helpful, but not a promise.
Common Reasons for Denial and How to Avoid Them
Denials are common, but often avoidable. The top reasons include:
- Insufficient Documentation: Missing or poor-quality X-rays, or a lack of detailed notes justifying the procedure.
- "Least Expensive Alternative Treatment" Clause: The insurer may only approve a less expensive option (e.g., a filling instead of a crown) if they deem it clinically acceptable.
- Administrative Errors: Incorrect patient information or procedure codes.
- Frequency Limitations: The plan may only cover a crown on the same tooth once every 5-7 years, for example.
Navigating the Appeals Process: Don't Take No for an Answer
Appeals Have a High Success Rate
Stunningly, while few patients appeal denials, data from Medicare Advantage shows that over 80% of appeals result in the initial denial being overturned. This highlights the importance of persistence.
If your request is denied, your dentist's office can submit a formal appeal. This usually involves providing more detailed clinical notes, higher-quality images, or peer-reviewed literature to support the medical necessity of the treatment. As a patient, you can also write a letter explaining how the condition affects your quality of life.
Your Role vs. Your Dentist's Role in the Process
This is a team effort. Your dental office is responsible for submitting the paperwork and providing the clinical justification. Your responsibility as the patient is to provide accurate insurance information, understand your plan's basic rules (like waiting periods), and communicate with your dentist about your treatment priorities.
Pro Tips for a Successful Pre-Authorization
- Be Proactive: Ask your dentist's office if pre-authorization is needed for your treatment plan.
- Ensure Quality Records: An experienced dental office will know how to submit high-quality, diagnostic X-rays and clear clinical notes.
- Stay Engaged: Follow up with your dental office on the status of the request and respond promptly if they need more information from you.
Conclusion: Taking Control of Your Dental Coverage
Pre-authorization is a standard part of modern dental insurance, designed to manage costs and ensure appropriate care. While it can seem like a hurdle, understanding the process empowers you to work effectively with your dental provider to secure the benefits you're entitled to. With faster review times and a high success rate for appeals, you can be confident that medically necessary treatment will be covered. Patience, clear communication, and persistence are your keys to successfully navigating the pre-authorization process.
FAQ: Your Top Questions on Dental Pre-Authorizations
Thanks to new CMS regulations effective in 2025, many plans (including Medicare Advantage) are now required to make a decision on standard pre-authorization requests within 7 calendar days. Previously, this could take up to 14 days or longer. However, timelines for commercial private plans can still vary, so it's always best to check with your specific provider.
No. A denial simply means your insurance company will not pay for the procedure. It is not a denial of the treatment itself. You always have the right to proceed with the recommended treatment by paying for it out-of-pocket. However, it is highly recommended to try the appeals process first.
While technically possible, it is not recommended. The submission requires specific clinical information, CDT procedure codes, and diagnostic records (like X-rays) that only your dental office can provide. The process is designed to be handled by the treating provider's administrative team, who are experienced in submitting the necessary information correctly.
No. In a true dental emergency (e.g., severe pain, swelling, or trauma), the priority is immediate care. Insurance companies do not require pre-authorization for emergency procedures. However, any follow-up treatment that is non-emergent (like a permanent crown or implant after an emergency extraction) will likely require pre-authorization.
